Frostbite
A cold day when the sun is at his highest, temperature below -30c are common in the Yukon
During our winter activities, we are exposed to the elements, especially the cold, which can be extreme here in the Yukon.
Over the course of my professional career, I’ve been fortunate to receive training in the prevention and treatment of frostbite and to work alongside leading specialists, like Dr. Emmanuel Cauchy, one of the world’s foremost experts on frostbite.
Despite this, I’ve personally experienced frostbite several times. Fortunately, thanks to what I learned , I was able to limit the consequences.
There is a lot of information out there about frostbite that isn’t always clear or accurate, and many persistent myths still exist. Many of you regularly ask me questions about this topic, so here is a short summary of the key things to know about frostbite.
Frostbite and frostnip: don’t confuse them
Frostbite is often confused with frostnip, which are an inflammation caused by cold exposure without tissue freezing. Even if frostnip could lead to frostbite, they are very different. Frostbite is much more serious: it can lead to cell death (necrosis) and, in severe cases to amputation.
Frostbite is a localized injury caused by direct exposure to temperatures below 0 °C for varying lengths of time, resulting in frozen tissue.
It mainly affects the extremities: fingers, toes, nose, and ears as well as exposed areas such as the cheeks.
Factors that increase the risk of frostbite
The main risk factors include:
- wind
- moisture
- high altitude
- inadequate cold-weather gear
- clothing that is too tight and restricts blood circulation
Exhaustion, dehydration, malnutrition, and certain medical conditions also increase the risk, as they reduce the body’s ability to protect itself from the cold.
Alcohol dilates blood vessels and increases heat loss—alcohol and cold do not mix well. Drug use can also impair awareness of environmental conditions.
How can you tell if you have frostbite?
The main clinical sign is loss of sensation, often without pain. The affected area may become completely numb, which is why frostbite can develop without being noticed.
Signs and symptoms of frostbite (before rewarming)
- cold limb
- complete numbness
- pale, waxy-looking skin
Be especially cautious if someone who was complaining about the cold while still exposed suddenly stops complaining and says they no longer feel pain.
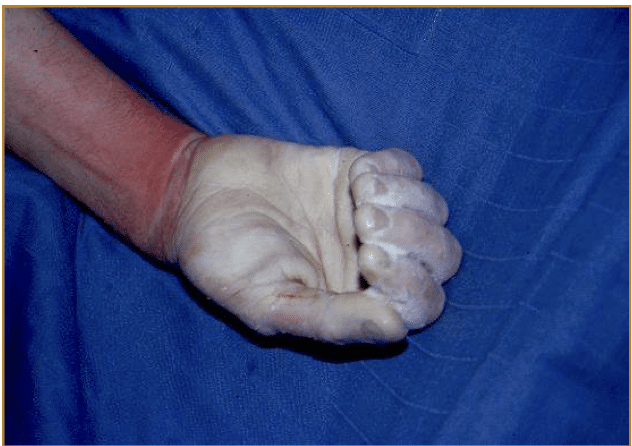
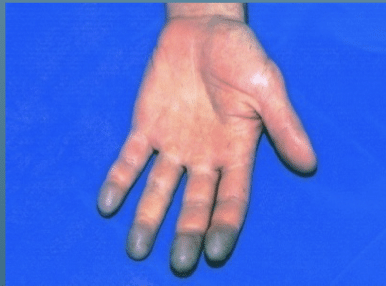
Severe frostbite before being rewarmed….and the same one a few hours after being rewarmed.
…and after a few days.
What to do – Prevention
Prevention is better than cure.
In the mountains and in cold conditions, check your extremities regularly. As long as you can feel the cold, it’s uncomfortable but reassuring there is no frostbite yet.
Move your fingers and toes often to detect any loss of sensation. If you notice numbness, it’s time to warm up.
- Hands: bring your fingers together inside your gloves and energetically swing your arms to send warm blood to your fingers.
- Feet: move your toes and vigorously swing your legs to improve blood flow.
If numbness is detected early, recovery is usually straightforward and you can continue frostbite are not there yet… typically, if it’s just for a few minutes, you’re good. But, If you wait too long and don’t notice it for more than 30 minutes it may be too late. In cold environments, I personally check at least every 10 minutes…and stop to warm up right away. When warming up your fingers or toes quickly, the rapide blood vessels dilatation and nerve reactivation can cause a throbbing pain, tingling and sometimes nausea because of the extreme pain…but it’s a good sign that the area is rewarming and is not subject to frostbite.
Warming up: yes, but the right way
If frostbite is suspected, the affected area must be warmed carefully.
⚠️ Never rewarm a frozen area if there is a risk it could freeze again.
Make sure you can keep the area warm afterward; otherwise, the damage can become much worse.
What you should definitely NOT do
Some myths are hard to kill, like rubbing frostbite with snow—this is wrong and dangerous. Treat the affected limb as if they were wounded or broken.
❌ Do not:
- rub, massage, or shake the affected area
- place the area near a direct heat source (fire, heating pad), which can cause burns because of a lack of sensation.
- smoke or use nicotine products, as they constrict blood vessels and worsen the injury
What to do if you think you have frostbite
- Remove any wet clothing from the affected area.
- Cover it with dry clothing and get to a warm place as soon as possible.
- Remove jewelry and tight clothing, as swelling may occur during thawing.
Rewarm the area:
- by immersing it in warm water (98.6–102.2 °F / 37–39 °C), or
- by applying warm compresses for 30–60 minutes.
Do not rub the area while rewarming. If warm water isn’t available, gently wrap the area in warm blankets or place it against your armpit, groin, or abdomen.
Continue warming until the skin regains a normal colour and feels warm and soft to the touch.
If you need to transport someone with frostbite, wrap them loosely in a blanket.
Pain and tingling during rewarming are normal. Over-the-counter pain relievers such as ibuprofen can help reduce inflammation and may limit further damage.
When in doubt, always consult a doctor—especially if numbness, tingling, or pain persists 24 hours after thawing, or if there are signs of infection such as swelling, warmth, fever, or discharge.
Severity and consequences of frostbite
It is very difficult, if not impossible to assess the severity of frostbite before the affected area has been fully rewarmed.
Only after rewarming, during the secondary phase, can frostbite be properly classified and its severity evaluated. The urgency of frostbite cannot be determined before rewarming.
Signs after rewarming
- skin that remains hard, waxy, and cold to the touch
- color changes (dark red or purple on light skin; dark purple, brown, or black on darker skin)
- dark blisters, sometimes filled with blood
- difficulty moving the affected areas, with possible clumsiness of the hands or feet
Secondary phase after rewarming
After rewarming, the secondary phase begins and is marked by clear clinical signs. As blood flow returns, fingers or toes may turn gray, bluish, or purplish.
The initial injury persists for 12–24 hours. Between 24 and 48 hours, blisters may appear—sometimes large and filled with blood. This is known as progressive secondary necrosis, which worsens the initial injury.
Preventing secondary necrosis is one of the main goals of modern frostbite treatment protocols.
Possible long-term consequences
Frostbite can result in:
- partial or persistent loss of sensation
- increased sensitivity to cold
- tissue necrosis that may require amputation
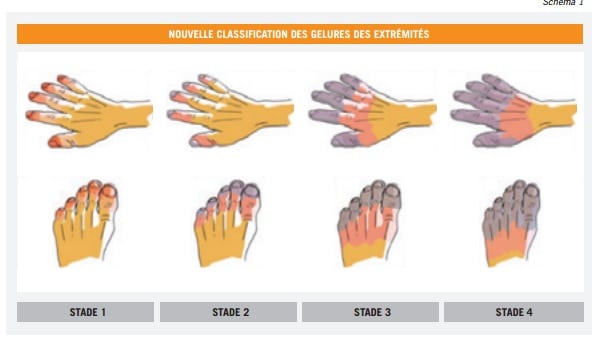
Several classification systems exist; the most useful ones help assess severity and the likelihood of permanent damage.
Stage 1
Gray or cyanotic lesion disappearing after rapid warming.
Stage 2
Persistent gray or cyanotic lesion on the first phalanx (joint) despite warming.
Stage 3
Persistent gray or cyanotic lesion going above on the middle phalanx (second joint) despite rapid warming.
Stage 4
Persistent gray or cyanotic lesion going above the wrist despite rapid warming.
Pictures from Emmanuel Cauchy.